Overview, Causes, & Risk Factors
Peptic ulcer disease occurs when the lining of the esophagus, stomach, or duodenum is worn away. The damage may be caused by stomach acid or other factors.
What is going on in the body?
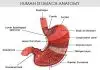
Peptic ulcer disease most commonly occurs in the upper part of the small intestine, called the duodenum. It also occurs in the stomach. Ulcers less commonly occur in the esophagus. The esophagus is the food tube that connects the mouth to the stomach.
What are the causes and risks of the condition?
Stomach acid is thought to play a role in causing peptic ulcer disease. A bacterial infection known as Haemophilus pylori may also be important in causing a person’s ulcer. Ulcers may also be caused by the use of certain pain medicines. Each of these factors breaks down the natural protective lining of the digestive tract. Inherited factors are also thought to play a role in ulcer formation.
Symptoms & Signs
What are the signs and symptoms of the condition?
Peptic ulcer disease causes no symptoms at all in some people. Common symptoms include:
Diagnosis & Tests
How is the condition diagnosed?
The medical history and physical examination may be enough to diagnose an ulcer. X-ray tests or endoscopy can confirm the diagnosis. Endoscopy is a procedure that involves putting a thin telescope into the mouth. This telescope can be moved down into the stomach and bowels. This procedure allows the doctor to directly see any ulcers that are present. The doctor may take samples of the stomach contents to test for H pylori infection.
Prevention & Expectations
What can be done to prevent the condition?
Prevention of peptic ulcer disease includes:
Certain conditions cause a high risk of developing peptic ulcer disease. People with these conditions may be given medicine to prevent ulcers. For example, burn victims are commonly given medicine to prevent ulcers.
What are the long-term effects of the condition?
Untreated peptic ulcer disease may cause a hole in the digestive tract. It may also cause bleeding, inflammation, or abnormal connections between abdominal organs.
What are the risks to others?
Peptic ulcer disease is not contagious, and poses no risk to others.
Treatment & Monitoring
What are the treatments for the condition?
Treatment of peptic ulcer disease depends on the cause. If aspirin or other medicines are the cause, then these medicines must be stopped. Smoking and alcohol should be stopped as well, because they can delay healing. Medicines are given to help protect the stomach lining and allow faster healing. Most of these medicines work by neutralizing stomach acid or preventing it from being made. If an infection with a bacteria called H pylori is present, antibiotics are given. Surgery may be needed for severe ulcers that bleed, don’t respond to medicine, or cause a hole in the gut.
What are the side effects of the treatments?
Medications used to treat peptic ulcers may cause allergic reactions or rash. Surgery can cause bleeding, infection, or allergic reaction to anesthesia.
What happens after treatment for the condition?
With proper diagnosis and treatment, peptic ulcer disease can often be cured. A cure means that there is complete healing of the ulcer. However, if ulcers are severe or complications occur, surgery may be needed in the future.
How is the condition monitored?
A follow-up X-ray test or endoscopy can confirm that an ulcer is healed. Endoscopy can rule out stomach cancer , which sometimes causes an ulcer. A breath test can confirm the cure of a bacterial infection. Any new or worsening symptoms should be reported to the healthcare provider.
Article type: xmedgeneral