Overview, Causes, & Risk Factors
Coronary heart disease, or CHD, refers to the narrowing of the coronary arteriesthat supply blood to the heart. CHD is aprogressive disease that increases the risk of heart attack and sudden death.
What is going on in the body?
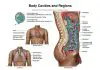
In order for the heart to pump as it should, the heart muscle needs a steadysupply of oxygen-rich blood. This blood is delivered by the coronaryarteries. Two main vessels branch out to supply blood to the entire muscle ofthe heart. The heart needs more oxygen during exercise and high levels of activity.Less is needed when the person is at rest.
Atherosclerosis means the fattydeposits that form under the inner lining of the blood vessels.When the coronary arteries become blocked, less blood can get through. Theblockage can be small, or it may be large enough to fully obstruct blood flow.Blockage can occur in one or many coronary arteries.
Small blockages may notalways affect the heart’s performance. The person may not have symptoms until the heart needs moreoxygen-rich blood than the arteries can supply. This commonly occurs duringexercise or other activity. The pain that results is called stable angina.
If a blockage is large, angina pain can occur with little or no activity. Thisis known as unstable angina. In thiscase, the flow of blood to the heart is so limited that the person cannotdo daily tasks without bringing on an angina attack. When the blood flowto an area of the heart is completely blocked, a heart attack occurs.
What are the causes and risks of the disease?
CHD affects people of all races. It can be caused by acombination of unhealthy lifestyle and genetics. Coronary risk factors that increase the risk of CHD are as follows:
Genetic factors that affect heart disease risk are beyond a person’s control. These include a strong family history of the following:
Symptoms & Signs
What are the signs and symptoms of the disease?
Symptoms of CHD vary widely and do not necessarily indicatethe severity of the condition. The classic indicator of CHD is angina, or chest pain. The pain may radiate to the neck,jaw, or left arm. It is often described as a crushing, burning, orsqueezing sensation. The person may also have shortness of breath.
Sometimes, a person may have no symptoms at all until he or she suffers a heart attack.
Diagnosis & Tests
How is the disease diagnosed?
The diagnosis of CHD starts with a medical history and physical exam. An electrocardiogram, or EKG, may show abnormalities. However, an EKG may be normalbetween attacks of angina.
A stress EKG is an EKG taken before, during,and after exercise. It is designed to bring on an attack of angina and recordthe changes that take place in the heart. Sometimes the person isinjected with a substance called thallium during the stress test. Specialpictures are then taken of the heart. The thallium scan can show areas of theheart that are damaged.
The most reliable test for diagnosing CHD is a cardiac catheterization. In this procedure,a thin hollow tube or catheter is placed into an artery in the leg or arm. Itis then passed through the artery and into the coronary artery. A contrastagent is injected into the tube. This allows the doctor to watch the blood flow throughthe heart and its arteries.
Other techniques that are being used to help in the diagnosis of CHD includestress echocardiograms and new generations of CT scans.
Prevention & Expectations
What can be done to prevent the disease?
Although family medical history or genetics can’t be changed, a person can lowerhis or her risk for developing CHD. Here are some steps that a person can take to lower his or her coronary risk factors:
Before menopause, women have some protection against heart disease. Experts believethis is due in part to the fact that they have adequate levels of estrogen in their bodies. This hormone may have a protective effect. Estrogen tends to raise HDL cholesterol, known as thegood cholesterol. It also lowers total cholesterol. There is no proof that estrogen replacement therapy has this same protective effect in a woman who has gone through menopause. Estrogen replacement therapy is a form of hormone replacement therapy, or HRT.
In fact, the latest recommendation from the American Heart Association, or AHA, does not advise starting HRT for the sole purpose of preventing heart disease. There is not enough data to support this. This same advisory issued by the AHA in 2001 recommends that women who already have heart disease should not be started on HRT. In fact, a recent study has even shown that if HRT is started after a woman has a heart attack, she may be at a higher risk for worsening of her angina, or having other serious cardiac complications.
What are the long-term effects of the disease?
CHD is a progressive disease that can lead to heart attack and sudden death.
What are the risks to others?
Coronary heart disease is not contagious. However, it does tend to run in families.
Treatment & Monitoring
What are the treatments for the disease?
Several types of medicines are often used together to reduce thesymptoms of stable angina caused by CHD.
Calcium channel blockers, such as diltiazem, nifedipine, or verapamil, have been used for more than 20years to open the coronary arteries and lower high blood pressure. However,two recent studies have found that people who take a calcium channel blockerhave a much higher incidence of complications than people taking othermedicines for high blood pressure. One study, for example, found that therisk of heart attack was 27% greater,and the risk of congestive heartfailure was 26% higher. The American Heart Association recommends thatpeople discuss risks and benefits of the medicine with the healthcareprovider.
Several surgical procedures can be used to reduce the symptoms of stable anginafrom coronary artery disease, such as:
What are the side effects of the treatments?
Side effects vary depending on the treatment used:
What happens after treatment for the disease?
Most people who have coronary heart disease are advised to start a regularexercise program. A person who has CHD should make every effort to reduce coronary risk factors. This may includesmoking cessation, control of otherdiseases such as diabetes and high blood pressure, and following a healthydiet for heart disease. Medicinesmay need to be adjusted to get the best response.
How is the disease monitored?
The person will have regular examinations and tests by the healthcare providerto check the progress of the coronary heart disease. Any new or worseningsymptoms should be reported to the healthcare provider.
Article type: xmedgeneral