Overview, Causes, & Risk Factors
A migraine is a moderate-to-severe headache affecting one or both sides of the head. An aura is an abnormal sensation which warns that a migraine is coming on.
What is going on in the body?
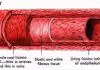
A migraine begins when cells in the central part of the brain become oversensitive to stimulation. The reason this happens is not known. A migraine trigger causes these cells to suddenly begin firing electrical impulses. This causes a chain reaction inside the brain. The impulses travel through the brain in a wave, similar to the way ripples spread across the water when a stone is thrown into a pond. This spreading electrical impulse causes the release of serotonin and other brain chemicals.
Serotonin causes changes in blood flow to the brain. When an impulse reaches the outermost part of the brain, it triggers the release of substance P and other chemicals. These chemicals contribute to the pain, inflammation, and increased sensitivity. The result is the throbbing pain you feel.
What are the causes and risks of the disease?
A migraine occurs when cells in the center of the brain become overly sensitive to stimulation. Factors that may trigger a migraine include the following:
Symptoms & Signs
What are the signs and symptoms of the disease?
A migraine with aura usually has the following characteristics:
An aura begins 5 to 30 minutes before the headache pain and may involve:
Diagnosis & Tests
How is the disease diagnosed?
Diagnosis of a migraine with aura begins with a medical history and physical exam. Rarely, the healthcare provider may order tests to rule out other problems.
Prevention & Expectations
What can be done to prevent the disease?
An individual can lower the risk for migraine with aura by identifying and avoiding triggers. People who are sensitive to tyramine, for example, should not drink red wine. Medicines used to prevent migraines include the following:
What are the long-term effects of the disease?
If the migraines are infrequent and mild, there are few long-term effects. If they are frequent and severe, they can greatly impair a person’s ability to function or work. Rarely, a migraine can cause a stroke.
What are the risks to others?
Migraines with aura are not contagious and pose no risk to others.
Treatment & Monitoring
What are the treatments for the disease?
Medicines used to relieve the symptoms of migraine with aura include:
Alternative and complementary therapies for migraine with aura include:
What are the side effects of the treatments?
Medicines used to treat migraine with aura may cause drowsiness, allergic reactions, or rebound headache. Rebound headaches are caused by regular use of pain medicines.
How is the disease monitored?
The individual may be asked to keep a headache diary to identify triggers and track the success of treatment. Any new or worsening symptoms should be reported to the healthcare provider.
Article type: xmedgeneral